
Hip arthrosis (coxarthrosis) is a degenerative disease of hip cartilage, which leads to continuous dysfunction of the joint and patient disability. More commonly, elderly patients can find joint disease of the hip joint, and men are more likely to get sick than women.
Classification of hip joint disease
There are two main types of the disease:
- Elementary-the onset of disease in the context of complete health;
- Secondary-in the context of inflammatory joint disease, after previous injury, and in the case of a congenital disorder of the development of the hip joint, which develops under dysplasia.
Causes of hip joint disease
According to the reasons for the development of hip joint disease, it is divided into the following types:
- Idiopathic-hip joint disease, which develops without a specific cause;
- Involution-arthropathy associated with age-related natural changes in the body, manifested in old age;
- Dysplasia (congenital)-arthropathy that develops in the joints against the background of congenital dysplasia;
- After infection-arthropathy that develops in the joints affected by rheumatoid arthritis, and due to some other infections;
- Post-traumatic-arthropathy, which develops due to traumatic injuries to the joints;
- Hormonal imbalance-hip joint disease, endocrine system disease or metabolic disorder caused by hormone therapy develops against the background;
- Blood vessels-the disease is caused by disturbances in the circulation of the joints;
- Heredity-developed due to the genetic characteristics of cartilage tissue development (usually combined with deformable osteoarthritis of other joints).
In addition, hip osteoarthritis may be the result of a violation of the body's motion biomechanics, which is usually accompanied by a curvature of the spine, an intervertebral hernia, or a bone defect in the lower extremity (for example, the shortening of one of the joints). they). Limpness or poor posture can put too much pressure on the hip joints, which can lead to hip joint disease. Another common cause of hip joint disease is inactivity. However, excessive physical activity (exercise or work) can also cause joint disease.
How does hip osteoarthritis behave?
First, patients with hip joint disease complain of hip joint pain. It is accompanied by limp, and over time, the thigh and buttocks muscles atrophy. The movement of the joints is accompanied by characteristic tightening; over time, the mobility of the joints decreases. The intensity of symptoms directly depends on the extent of the disease.
Hip joint disease 1 degree
The initial stage of the disease is mild pain, which may be troublesome in the morning or after a lot of physical exertion on the joints. You may also notice the weather sensitivity of the affected joints, which manifests as pain when the weather changes. The patient may notice morning stiffness of the joints, which disappears after exercise and warms up slightly.
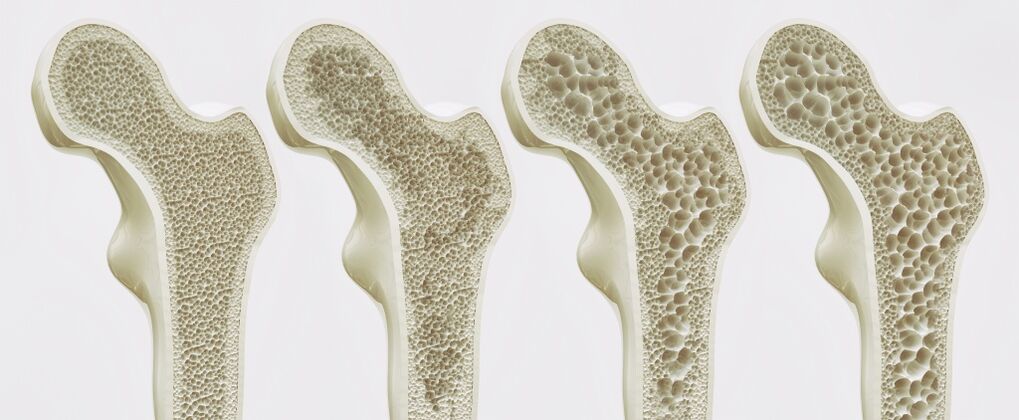
The radiological changes are minimal-the joint space may narrow slightly, and the cartilage covering the femoral head may become thinner.
Second degree hip joint disease
At this stage of the disease, the intensity of the pain increases slightly, and the pain radiates to the groin and knees. Misdiagnosed cases of hip joint disease related to pain radiating to the knee joint and popliteal ligament are not uncommon. Pain not only starts to appear after physical exertion, but also when resting. During the movement of the limbs, the joints will make foreign sounds (clicks, creaks). The range of motion in the joints is significantly reduced, especially for rotational (circular) motions, the biomechanics of the motion in the joints are impaired, so its function is reduced. Joint pain and decreased mobility can cause slight claudication, which in turn leads to moderate atrophy of the gluteal muscles on the side of the affected joint.
On the X-ray film, it can be seen that the joint space is reduced by one-third of the normal width, the cartilage is significantly thinned, there is no cartilage in some areas, osteophytes appear on the articular surface, the femoral head is deformed, and its upward displacement.
Hip joint disease grade 3
At this stage of the disease, the pain becomes persistent, including at night, and analgesics are difficult to relieve. The range of motion of the joint is minimized, and the biomechanics of the joint is significantly impaired. The slightest movement is accompanied by crepitus, claudication becomes obvious, the pelvis is noticeably twisted, and the limb on the side of the affected joint is shortened. Atrophy of the gluteal and femoral muscles on the affected side. Due to severe claudication, patients are usually unable to move independently without using a cane or support.
X-ray examination showed obvious deformation of the femoral head and thickening of the femoral neck. The articular surface is covered by bone hyperplasia, and the joint space is reduced to almost non-existent.
Diagnosis of hip joint disease
The diagnostic measures are first to interview patients and examine them, perform some laboratory tests, and then use special instrument technology to confirm the diagnosis. The following methods are considered the most useful methods today:
- X-ray inspection——Allows you to view the contour of the joint surface, whether there is bone growth on it, to determine whether there is a femoral head deformity and the width of the joint gap;
- Joint ultrasoundNot only can check the joint surface, but also identify the dystrophic changes of the joint ligaments;
- Computed tomography (CT)-The layer-by-layer image of X-ray type can be obtained, but it is clearer and larger;
- Magnetic resonance imaging (MRI)-Allows you to study the state of joint structures, articular surfaces, bones and ligaments in a highly visual manner. Currently, it is considered the most advanced diagnostic method.
Hip joint disease treatment
Taking into account the stage of the disease, the most effective is the comprehensive treatment of hip joint disease. It should be remembered: the sooner treatment is started, the more likely it is to avoid disease progression, inability of the patient to move, and incapacity to work. Therefore, even if you have mild joint discomfort, seemingly insignificant pain, stiffness, and joint allergies, you need to consult an orthopedic doctor for examination, confirm the diagnosis and prescribe a treatment plan. The cartilage tissue has not recovered, so it is best not to wait until the moment when the damage is serious, but to start treatment at the stage of cartilage dystrophy until it undergoes irreversible changes.

The scope of treatment depends on the stage of the disease. Therefore, for first-degree hip joint disease, use non-narcotic analgesics and non-steroidal anti-inflammatory drugs-they can eliminate pain syndromes and eliminate inflammation in joint tissues, preventing further damage to their tissues. Since the pain syndrome and inflammation are not severe at this stage, there is no need for long-term use of such drugs. Usually, the use of local means is sufficient-ointment, a gel containing non-steroidal anti-inflammatory drugs. At this stage, it is more important to ensure the normalization of the metabolic process in the cartilage tissue to minimize its degradation. For this purpose, drugs of the cartilage protective agent group are used. Their task is to restore the metabolism of cartilage tissue cells, thereby improving the nutrition of the joints and reducing the intensity of inflammation. For example, in the treatment of hip joint disease, a cartilage protection drug has proven its effect, and its active substance is the source of natural components of healthy cartilage tissue. It stimulates the production of proteoglycan, the most important structural component in cartilage, and prevents the destruction of cartilage tissue.
The comprehensive treatment of second- and third-degree hip arthropathy is much more difficult: the cartilage has been significantly damaged, the articular surface is exposed, and a large number of osteophytes are formed on it, which hinders the normal movement of the joint. At this stage, only symptomatic treatment is available, which can reduce joint pain and slow down the process of cartilage destruction. The pain during this period is severe, and it is relieved with analgesics and non-steroidal anti-inflammatory drugs. The best way is to use a combination of topical drugs (ointments, creams) and systemic dosage forms (tablets, injections).
During the deterioration of the disease, no matter what stage it is, the load on the joints should be reduced as much as possible to avoid further damage to the cartilage. During remission, in addition to taking chondroprotective agents to normalize the metabolic process of cartilage tissue, exercise therapy, massage, and exercise therapy are also recommended. They provide reasonable load for joints, prevent their fixation and the deposition of mineral salts in joint tissues and ligaments, and stimulate microcirculation. Exercise therapy is also very important for the general state of the body: bioactive substances are produced during exercise, which increase mood and overall well-being-endorphins and serotonin.
Proper nutrition plays an important role in the comprehensive treatment of hip joint disease. The patient's diet should be complete, rich in plant and animal protein, fiber, and vitamins. Proper nutrition is not only important for stimulating joint regeneration, but also for keeping the patient's weight within a normal range. Being overweight is an additional burden on diseased joints and a factor in disease progression.
In the remission phase, physical therapy methods have proven their effectiveness-electrophoresis, mud therapy, ultrasound and magnetic therapy. In addition, attention was paid to the effectiveness of biological and mechanical methods for the treatment of hip joint disease. Among the biological methods, the most popular is leech therapy (leech therapy), which provides blood dilution and stimulates the capillary microcirculation in the joints and surrounding muscles, thereby preventing their shrinking process. Mechanical methods include joint traction to relieve excessive pressure on the affected joints and acupuncture. However, it should be remembered that the physical, mechanical, and biological methods of treating hip joint disease can only be used during remission. As the disease worsens, their use is fraught with the progression of inflammation and destruction of cartilage tissue.
If the conservative method of treating hip joint disease does not work, the patient may be offered surgical treatment-arthroplasty and joint replacement. The first variant of surgery involves restoring the mobility of the joint due to the plastic of its own tissue, and the second variant-replacing the joint surface with an endoprosthesis-the mechanical joint. Surgical intervention can allow you to restore the mobility of the joints and the ability of the patient to work.
Prevent hip joint disease
Preventive measures are reduced to taking chondroprotective agents, proper nutrition and reasonable pressure on the joints, especially for those who exercise or physical labor.
Hip joint disease is a serious disease that can deprive patients of the ability to move independently. By seeking medical help in time when the joints experience discomfort for the first time, disability can be avoided and effective pathological comprehensive treatment can be received from the initial stage.



































